Thank you to everyone for reaching out and checking in with me, Andrew, other family members, and the close friends who have been on-call for us these last few weeks. It’s been a hectic, busy, and an overwhelming time — especially the last week or so.
During the first two weeks post-radiation, I was able to recuperate with a relative lack of chaos. Still, even in the somewhat stable days, many moving parts were being coordinated and researched. I was doing that with a brain that still isn’t cognitively 100% and all of the other side effects I wrote about in the last post.
But I have made progress, logistics are falling into place now, and a plan is coming together that makes sense and gives me some hope. Let’s get into it! The good, the bad, and the ugly…except not in that order.
The Ugly — When I was first told about Leptomeningeal Disease (LMD), I didn’t fully comprehend what was being thrown my way. It was entirely out of left field, and I have learned throughout August that LMD is rare — only 3-5% of all breast cancers metastasize this way, and in my subtype of breast cancer (hormone positive, HER2-), this is even rarer. We are dealing with a unicorn here, not in a good way. LMD is extremely serious and dangerous. The rapid response to getting my treatment started was appropriate for a reason. My personal LMD is also acting exceptionally aggressively, and we don’t know why. If we can’t get control of this disease quickly, this is the worst-case scenario. We have now jumped the queue on other treatment options that work well in other parts of the body to mainly focus on the LMD because I am symptomatic, and it’s spreading.
The Bad — it’s spreading. Yeah, after whole-brain radiation and a dose of Doxil, I continued to have symptoms. My feet continue to experience numbness and tingling, which isn’t resolving. I bought myself a pair of “stability-sneakers” to walk more efficiently and comfortably. At least they aren’t wicked ugly! haha! I also continue to feel off balance and have weakness in my legs and arms. My doctors have said these symptoms are the cancer taking root in my spinal cord, not the effects of the steroids or treatment. The steroids cause my jitters and cloudy mind, but anything else is really cancer itself. The scan I had two Fridays ago confirmed that the LMD was more visible and that the cancer now has left lesions on the cord itself. Not good.


The Good — Now, here is where the plan and the hope come in. When considering treatments when first given the LMD diagnosis, two types of radiation were presented to me. Traditional X-ray or photon radiation to the whole-brain or proton radiation therapy. Conventional whole-brain radiation has been the standard of care for a long time and is a good option when you want to treat the whole brain because the radiation beams will not hit any other organs and will only impact the brain. Cool cool, that makes sense. But when we are talking about radiating the spinal cord, if traditional radiation is used, it goes beyond the cord, and the beams will hit the heart, lungs, digestive organs, bladder, etc. Some severe side effects come along with that, which is why traditional radiation to the spine isn’t preferred.
Proton therapy, on the other hand, has this unique ability to stop radiating at the tissue that you want it to treat, avoiding other things like those organs we want to protect. It’s very promising. Proton therapy also has a better efficacy with LMD, potentially extending my life by months, not weeks, and offering a better quality of life. So why didn’t I do proton therapy to start with? It’s not as widely available, it takes longer to map/simulate, and insurance always denies it before approving it, so that process takes TIME. I didn’t have time on my side when I was given the news. Remember, I said that if left untreated, LMD can be deadly within weeks.
There are not a lot of proton centers around the USA. There is one at Mass General (MGH) in Boston, but they refused to take me on as a patient because they don’t like to split up brain and cord treatment, and their list of waiting patients is quite long. So, I started digging elsewhere. I found that there are less than 40 centers in the country that can do proton therapy, and since this is me, I wanted to look at the best ones first. My radiation oncologist said if I could find a place to take me on as a patient, he would support it, but if I couldn’t, we couldn’t wait much longer, and my only option would be doing traditional radiation to the spine next week.
I have reached out to four centers, and eventually, one in New Jersey worked quickly and said YES to taking me on as a patient. The center is called ProCure and is in Somerset, NJ. They are given a lot of overflow patients from Memorial Sloan Kettering (which, like MGH, has a long wait list). They have been great about working with my insurance and expediting my case. The whole process has been overwhelming yet smooth with them, making me feel like my efforts are moving me in the right direction. This puzzle piece is coming together.
Right now, the radiation plan is that I will go down to NJ this coming week with my sister-in-law on Tuesday/Wednesday via train (I still can’t fly as my seizure risk is still thought to be elevated). This initial appointment will be for mapping/planning/radiation simulation. After the doctors collect all the information they need, they can do all of the calculations and get me started on 10 daily treatments beginning Monday or Tuesday of the following week. I will need to set up shop in NJ for 5 days at a time, and I’ll come home the weekend in between.
It’s a huge sacrifice for my family to support me in this, and I am so grateful for their willingness to see the hope this treatment offers, too. Andrew will remain in NH with the kids. My in-laws and close friends have been pitching in with childcare, rides, and support. We added dates to the meal train to help Andrew, too. One of my sisters and one of my brothers will split their time in NJ with me, so I have accompaniment. My mom is coming to NH to help out as well. I cannot express enough how much this all means to me. This isn’t for the faint of heart. In addition to my own Cancerland stuff, we still have a very active and full life, including my son starting a new school this fall, his 9th birthday, fall sports, music, and other activities. It’s A LOT, A LOT – ALOT.


Radiation is targeted, though; we must treat my body systemically, too. Doxil was clearly not working because the LMD grew, and according to my CT scan done last Thursday, the lesions on my liver, that were improving on Taxol, also started to grow again. Out with Doxil and in with something new.
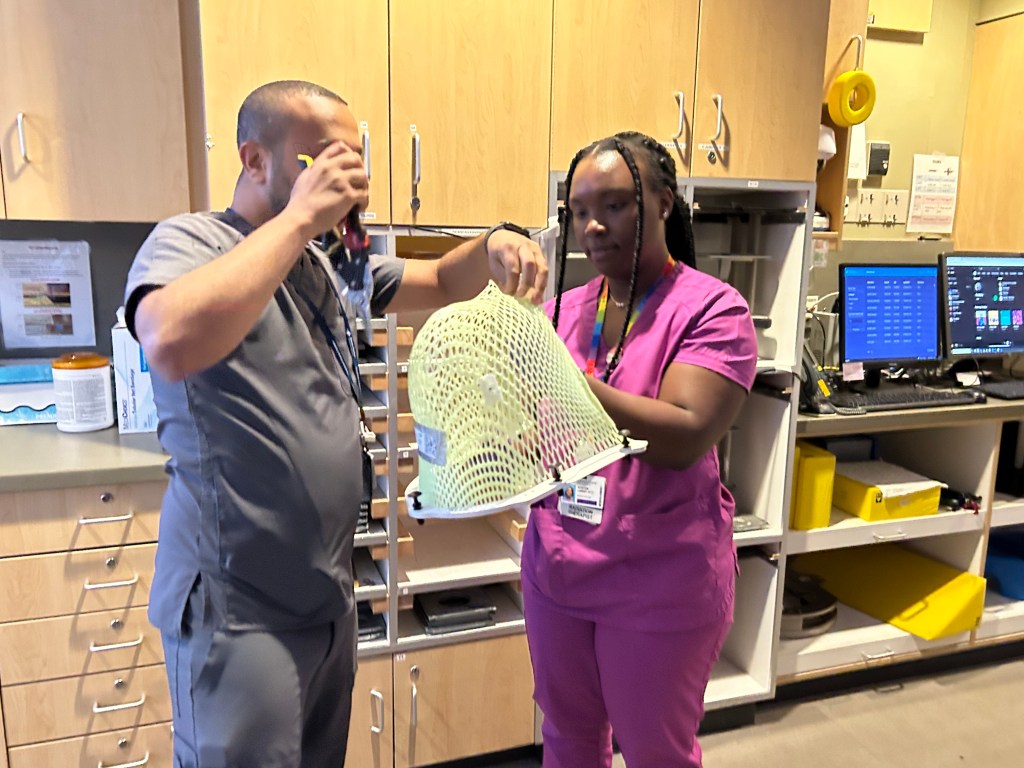
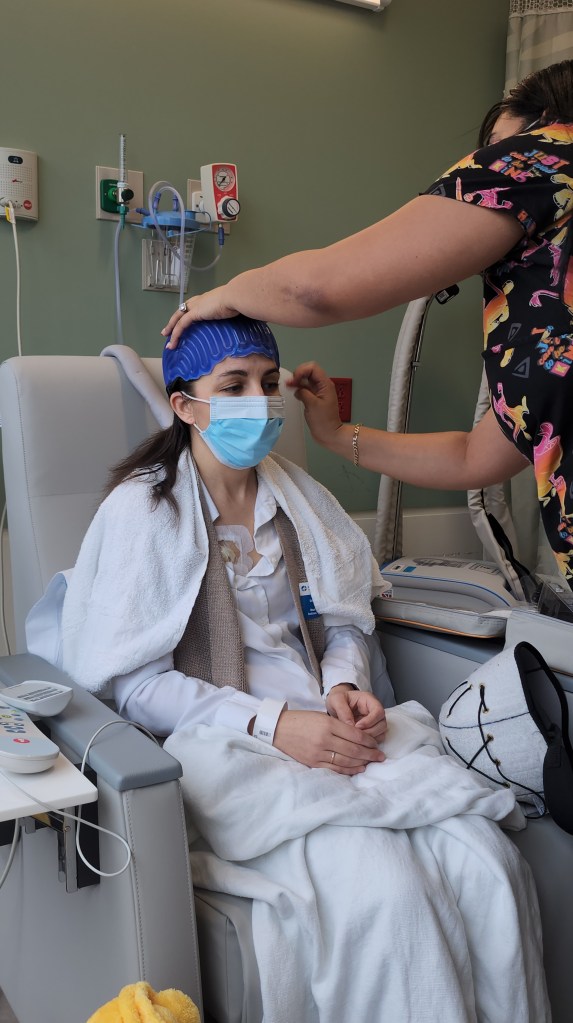
My oncologist wanted to start me on a new chemo before radiation. Still, timing is tricky because I needed about a week of “wash-out” between chemo and radiation so that I wasn’t miserable with side effects. I was scheduled to get Sacituzumab (AKA Saci or Trodelvy) this Thursday, but I got a call yesterday saying they could fit me in today (Sunday) for a treatment. I jumped at the opportunity and received my first dose of Saci.
The chemo itself is a cousin of Enhertu (was on from January 2023 to May 2023), but it has shown to be a very effective drug at crossing the blood-brain barrier and hitting really aggressive breast cancer. It’s a heavy hitter though, and requires many pre-meds. I expect to have side effects around day 3-4 and last a few days. I am told I can expect nausea, maybe vomiting, diarrhea, fatigue, hair won’t be coming back on this one, low white blood counts, etc. You know, all of the things we think of come along with traditional IV chemotherapy.
If you’re still here reading this, I appreciate it. I will always try to text or message you back if you reach out; it might take a day or two. Please continue to send those prayers and good vibes my way. I am not asking for a miracle, just manageable side effects and a little more time with my loved ones.
Sending you all a big Hannah Hug tonight!