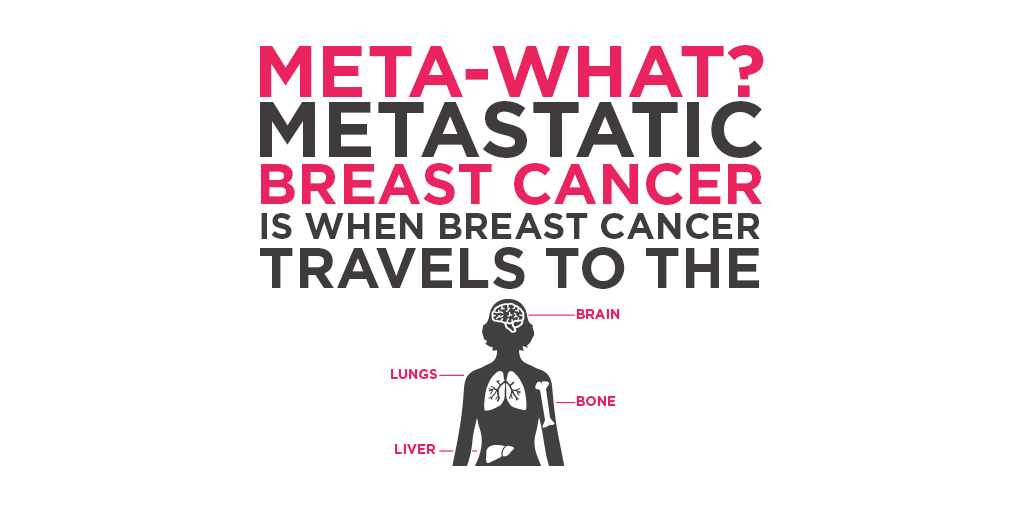
At the beginning of this shitty ordeal, I had lots of imaging done. We determined that there is cancer in my bones (skull, ribs, vertebrae, and sternum), no cancer in my liver (benign spots only), that there are cysts on my ovaries (benign likely too), and there are very TINY spots in my lungs (also likely benign, but too small to know for sure or to biopsy). I was relieved in some ways because having bone-only mets is the best of a crappy situation. Those with bone-only mets usually do better in the long run.
After 4 weeks I was given another CT scan (this one being for the start of the trial). In that period of time the spots on my lungs grew — 3mm each. That much growth in just a few short weeks led my oncologist to believe that those spots on my lungs are actually metastatic lesions. Shit. Not good news. The good news in this situation is that my treatment doesn’t change. I get to still be in the trial.

When I went in last week to get the second infusion I also had blood work done, as I do two out of every three weeks. This brought some more unfortunate news. I expected my blood counts to be low as that’s one of the more common side effects to the medication I am on. Sure enough, yup, my blood counts were low. But not too low that I couldn’t have treatment. What surprised me was that my thyroid numbers were off the charts. My thyroid was in a state of hyperactivity.
Immunotherapy is amazing. Immunotherapy activates part of my immune system so that my own body can find cancer and kill it. But it can also cause my immune system to attack normally functioning organs, causing some pretty serious side effects. It was (and still is) a risk I was willing to take. My oncologist said that because I am so closely monitored, they would likely see any serious side effects before I would notice symptoms.
Well, that is what is happening with my thyroid. I thought I would have many more cycles under my belt before something like this showed up. Unfortunately, it happened after my first cycle. Immunotherapy is causing this issue. My provider is going to continue to monitor my thyroid numbers, but she predicts that I will eventually (sometime soon) have a hypoactive thyroid. When that fluctuation happens I will be referred to an endocrinologist. Thyroid issues are generally well managed with a daily medication, so I am told.
These are the kinds of things that most people with MBC get to figure out. I have to ask myself questions like: do I want to have the chance to live longer, but the tradeoff is that I might have other diseases or issues to deal with (caused by the treatment for MBC)? Well, if those issues are well managed would I trade that for the standard of care for MBC (which isn’t well managed)? What if those diseases amount to a worse quality of life than that of MBC? What if the treatment doesn’t work for MBC and I am left with serious side effects from treatment? It’s emotionally draining, and it’s hard to know what the right choice is.
But enough with the bad news! One super AMAZING thing that has happened since I was diagnosed is that the tumor on my sternum feels MUCH smaller than it did 4 weeks ago. I have more imaging on December 2, with results on December 6. This will hopefully give us a good idea of what has been happening in my body since the start of treatment. Fingers crossed it really is shrinking and isn’t hiding behind my sternum and that the spots on my lungs and bones are also shrinking.