As you may have read on another blog post, I have been having mixed results with this drug. As you can imagine, it’s frustrating that the cancer isn’t having a complete response. Treatment is hard, emotionally and physically, and it takes a toll. To not have great results, when it feels like it’s costing so much already, can be very disheartening, disappointing, and frustrating. That being said, stable is stable is stable… words I so desperately want to hear each time I go in for an appointment.
Sometimes I wonder if y’all are thinking why isn’t she jumping for joy for stable? Here’s why: right now, for me, stable is “mixed.” There is growth AND there is shrinkage or stability, but it’s not a homogeneous response. The heterogeneous nature of the response leaves me feeling very vulnerable. It feels like I am standing on the edge of a cliff and if a really big gust of wind came up behind me I could be swept away into the valley below. But on the other hand if the wind came at my front it could push me right back into safety. My liver lesions could turn on me at any moment and I could be kicked off this drug at any time.
I don’t have years of experience with mixed results, so I am still learning how to sit with that news. When I was on my first line of treatment in the MBC setting the cancer in my body shrank and shrank and shrank. I got to the place of no evidence of active disease (NEAD) and stayed there for a long time. I felt relatively well for a long time too. And I knew starting IV chemo would be a big challenge to my life, my body, and my mind.
NO LIGHT AT THE END OF THE TUNNEL
This wishy-washy place I am at right now is extremely hard to handle mentally. I am back to worrying about every little thing that feels off in my body, every hurt, every headache, every breath that feels difficult, etc. I know my body pretty well, but I don’t like to worry about it all the time. Who does? I remind myself often that I can tell cancer “not today” and I find joy in lots of small moments in my day. But below is a small glimpse into what I have to dig deep through to get to the joy.
In 2016 when I had my first round of IV chemo, I counted down from eight total chemo treatments. Every two weeks I got to cross another treatment off my list, which felt like moving towards the light at the end of the tunnel… a cure, an obstacle I overcame, the continuation of the rest of my life! I don’t have that count-down to the end anymore. This time I am counting up, hoping and praying that every three weeks I will actually be able to receive treatment, one more time. So far I have been able to receive five treatments. There is no lifetime limit on how many Enhertu infusions a patient can get because either the drug stops working or the side effects/adverse events are too big, too much for a patient’s body to tolerate. Remember, if a patient is moved off the drug it’s not their fault, they haven’t lost a battle. The drug has failed them. And even though I believe that with every fiber of my being, it’s really hard not to question: What could I have done differently if this drug gets taken away from me?
THE CYCLE
Let’s talk about what I feel every three weeks. We call these cycles for a reason. It’s cyclical and I am getting used to knowing what to expect for the most part. At my last treatment I realized I was starting to have a psychosomatic response before even receiving the medication in my IV line. I started to feel nauseous as soon as I hit the infusion suite. Not sure what I can do about that, so I dealt with it the same way I deal with nausea when I am not in the infusion suite: ginger chews, mint gum, and some slow breaths.
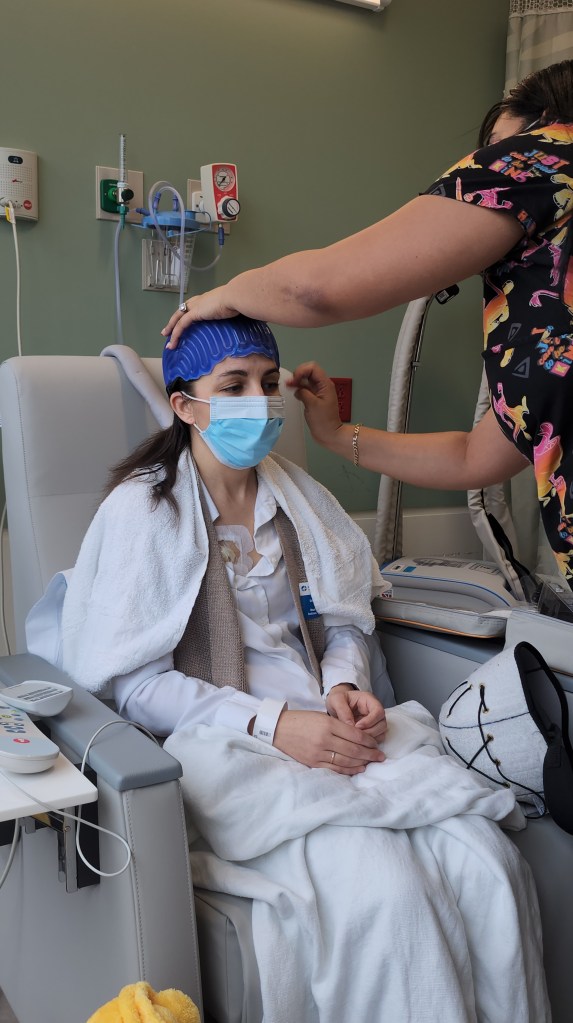
Since I am cold capping still, I get a dose of Ativan and ibuprofen to help take the edge off the freezing head. Before the chemo infusion I get pre-treated with anti-nausea drugs. I am currently receiving Aloxi, Emend, and Dexamethasone. These three medications will give me about three days of anti-nausea protection, but they aren’t perfect. I actually still feel pretty nauseous at times, I just don’t vomit.
I am usually very sleepy for the first 12hrs or so after the infusion, then the lasting effects of the Dexamethasone (a steroid) kicks in and I am in a weird awake, but exhausted state for 24hrs. I do a lot of sitting, napping, and watch TV. My head isn’t right. I am often grumpy and spacey at the same time. On day 3 (which is usually Sunday since I have been having infusions on Thursdays) I am in bed most of the day. It’s the day my body is in the most pain (deep bone pain), I feel the most nauseous, the most exhausted, and just the worst all around. I wake up on Monday feeling WAY better, but still fuzzy and not quite like myself. Tuesday I am generally back to doing normal activities, and by Thursday (a whole week out from the infusion) I am back and ready to rock and roll into regular life.
Not everyone that gets Enhertu feels this same way. We all have our own experience.
It’s hard to express the challenge if having 4ish days, every three weeks where I feel incapable of being normal or doing normal Hannah things. I am not one to just sit and relax easily. I don’t like pushing my normal activities onto anyone else. And I definitely don’t want to miss something because of chemo recovery, that’s just not fair! It’s hard on my kids because I am not in normal mom mode, and I am more obviously “sick.” It’s hard on my husband because he shoulders so much more in the lead up to and post infusion. Then once I am back on my feet again I put all of my energy into getting back up and running. The start and stop nature of the cycle is challenging for coordinating meetings, appointments that aren’t cancer related, play dates, activities for our family, etc. No one else’s schedule runs like that.
I have been making lists of projects that I can do while recovering and lists of things I can do when I am not in recovery mode. In my brain I work in these three week cycles: 1 week down, 2 weeks up. If you ever reach out to my during that week I am likely to either forget that we talked or forget to respond. If we make plans, make sure you remind me to write it down.
OTHER SIDE EFFECTS
There are the side effects that are more cumulative too. Like I alluded to above, my brain just doesn’t work quite the same as it did before I had Enhertu. There’s chemo fog that lasts 3-4 days. Then there is chemo brain which makes me feel like I have chemo induced ADHD (this is not a real thing btw, I made it up). I have trouble focusing, reading for more than a few minutes is a real challenge, my word recall is terrible, I walk into rooms and completely forget why I am there, if I don’t write things down I forget them almost immediately, I have been more impulsive, and more than a few times I have had racing thoughts I cannot slow down even though there is no reason for the panic. I am seeing a psychiatrist next week to talk about these changes.
Two other things I have to be very cognizant of, although I haven’t had issues with them as of yet, are issues of the heart and lungs. Enhertu can be cardio toxic meaning that it can cause heart issues. I have echocardiograms every three months to monitor this issue. The second issue, and probably more likely to occur than cardio toxicity, is something called interstitial lung disease (ILD). This is a fancy way of saying lung inflammation. This is a fairly common and could be a rapidly harmful side effect. Signs of ILD are quick onset of a dry cough or shortness of breath. If I have either of these symptoms, day or night, I have to call my oncologist right way. If someone develops ILD they would have to take a break from Enhertu and in many cases patients are pulled off the drug all together. Those are just another two things I have to think about every day.