Let me take you back two years. In 2016 I was diagnosed with Stage 1 Invasive Ductal Carcinoma (IDC). My cancer was small in size but aggressive in nature. My tumor was ER/PR+ meaning that my cancer cells really liked estrogen and to a lesser extent progesterone. I chose a lumpectomy, aggressive chemotherapy, and radiation. After active treatment, I opted to take Tamoxifen (a daily oral medication that blocks the uptake of estrogen in breast cells). At this point, my body was still making estrogen, but the tamoxifen was supposed to be preventing the absorption of estrogen in my cells.
Now fast forward to 2018: In July I found a small lump on my sternum. We were traveling abroad, and I knew I had an OBGYN appointment scheduled for when we got home. I figured this could wait a couple of weeks. After two weeks the lump disappeared. Wasn’t palpable. Cancer doesn’t appear and then disappear. I was feeling pretty good about this. My OBGYN NP also couldn’t palpate the lump. So I left her office with orders to call if the lump reappeared. A week later, it was back. I took a video of my chest and emailed it to my nurse practitioner. The fantastic woman was on vacation and got back to me right away. She wanted imaging done to figure out what this mass was.
A call to my oncologist office and one ultrasound later, we were still perplexed. An MRI would be needed next. The day I had the MRI I decided to get my images on a disc and look at them at home. What I saw scared me. I saw a tumor that wasn’t just on my sternum but growing behind my sternum, into my chest cavity. My oncology NP called me the next day and told me it appeared malignant, and there was more. A spot on my spine also looked concerning. I would need a biopsy.
A biopsy, followed by a bone scan, and a CT scan led to what I most feared when I was an “early stager.” I am metastatic. I have metastatic breast cancer. Thirty percent of early stagers (those stages I-III) will become metastatic. I was in that thirty percent.
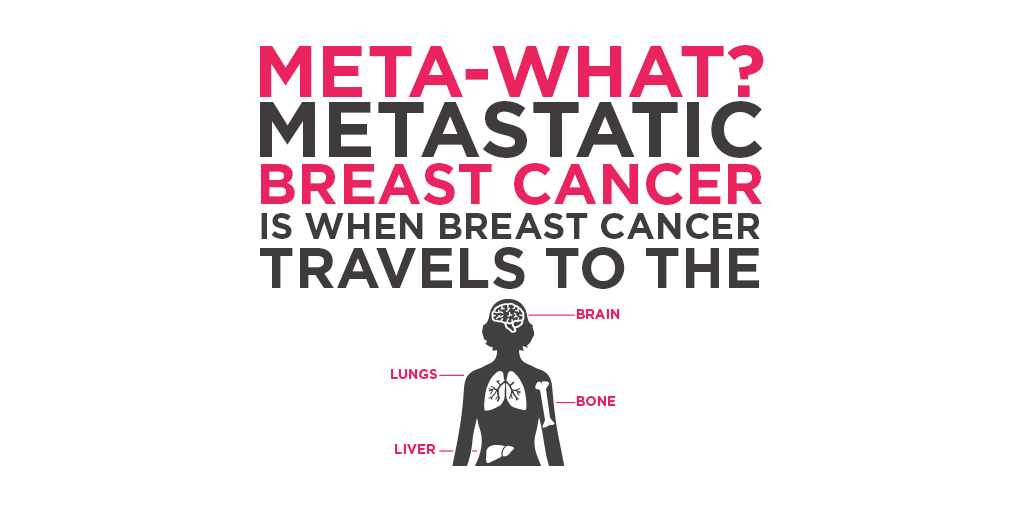
The scans showed that breast cancer is in my sternum, spine, skull, and ribs. When breast cancer leaves the breast and travels to distant parts of the body, this doesn’t mean the cancer becomes bone cancer, or liver cancer, etc. This is still breast cancer, but it has traveled to my bones.

